Software solution to drug shortages
Deciding how to fix health care is hard enough. But when huge problems I didn’t even know were problems come to light, it makes me wonder how we can ever hope to change. Then again, every problem is a solution waiting for someone to take charge.
In this case, drug shortages could be studied and solved through smart tracking software run by a national health organization or on a smaller scale within a hospital system.
Problem
In today’s New York Times, Sheri Fink detailed drug shortages and rationing that are apparently a fact of medicine.
The American Society of Health-System Pharmacists currently lists inadequate supplies of more than 150 drugs and therapeutics, for reasons ranging from manufacturing problems to federal safety crackdowns to drugmakers abandoning low-profit products.
And those 150 drugs seem to include many commonly used ones since most cancer doctors were unable to properly care for patients due to the problem:
In a survey of cancer doctors conducted in 2012 and 2013, 83 percent of respondents who regularly prescribed cancer drugs reported having been unable to provide the preferred chemotherapy agent at least once during the previous six months. More than a third of them said they had to delay treatment “and make difficult choices about which patients to exclude,” according to a letter published in The New England Journal of Medicine.
Perhaps I shouldn’t feel ignorant for having been blissfully unaware of this. It seems most of the time a shortage of a lifesaving drug deprives a patient of a fair chance of not dying, not even the patient or family is told.
Doctors and hospitals often do not tell patients about shortages and the resulting rationing because they do not want them to worry, especially when alternative drugs are available, or because they feel it would stir up too much anger.
Movement
The Cleveland Clinic has gone so far as to manufacture their own drugs if necessary, and they have been vocal about the problem, which I find admirable. The article mentions several hospitals and organizations developing guidelines for rationing in an effort to mitigate the damage, and there seems to be agreement patients should be informed. (This would be automatic, by the way, if all hospitals followed the lead of Paul Uhlig and included the patients and families in all planning meetings.)
Doctors proposed systemwide solutions:
The vagaries in distribution and inconsistencies in rationing have led to calls for change. Doctors and others have suggested the creation of a clearinghouse of scarce drugs and voluntary sharing to promote equitable access for patients. Others argue that there should be a registry of patients given nonstandard treatments so the results can be tracked.
The government emphasizes better preparedness:
Dr. Lurie, the federal health official in charge of emergency preparedness and response, said that the government was working to encourage hospitals to conserve and substitute drugs to avoid a crisis and trying to fill gaps in manufacturing. Steps taken by the Food and Drug Administration have also helped reduce the number of shortages, she said.
Solutions?
I was hoping for more detail on the supply problem itself. Without a clear understanding of the core issues and knowledge of how sticky they are, there is little hope any proposed solution would do more than ease symptoms.
- Manufacturing
- How often is each drug out of stock?
- What quantity of drug sales are thereby not realized?
- What portion of the total annual supply does that represent?
- Is this something the manufacturers would be more likely to prevent if they knew the extent of downstream consequences, or if public pressure were applied?
- If it’s just a problem of financial incentives, is there potential to solve the problem by:
- raising the drug prices?
- government subsidies for production?
- a nonprofit manufacturer taking over or acting as a backup supplier?
- Distribution and inventory management
- Could hospitals reasonably bridge these gaps through stockpiling, or does that just exacerbate the problem for other hospitals in the short term?
- Could hospitals reasonably bridge these gaps through sharing, or are the drugs needed hard to predict till the situation is already life or death?
- Could existing retail inventory management tools be utilized?
- Could existing business intelligence and predictive analytics software be utilized?
- Usage
- How many patients does this affect?
- How many are able to be treated with other drugs?
- How many deaths are likely preventable?
- What other burdens does substitution or lack of treatment put on the system, such as extra surgeries, etc.?
That said, it seems to me the haphazard approach is not working, and anything we can do to foster communication and systemwide consistency and tracking would be steps in the right direction.
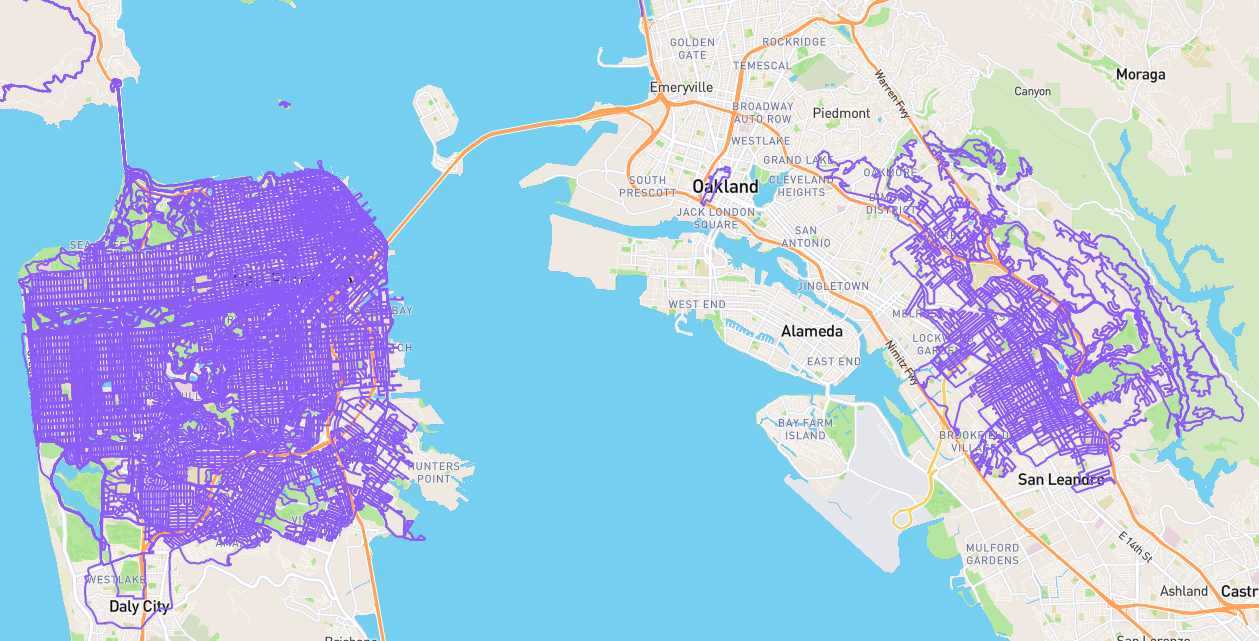
Provided a suitable solution doesn’t already exist, I would love to see the “clearinghouse of scarce drugs and voluntary sharing” idea combined with the “registry of patients given nonstandard treatments” in a unified software product. If the supply problem is small enough, perhaps sharing would get us 80 percent there with 20 percent of the effort. Further, I see potential for a fancy machine learning based predictive analysis to both understand how much stockpile is needed to weather a shortage and to help schedule surgeries and procedures that could reasonably be postponed. The system could track drug orders and usage on a per hospital basis, and shortages and associated causes could be studied for patterns, associations with predictable events, etc. Finally, when there is a shortage, hospitals could log all the adjustments they needed to make, facilitating followup and better understanding the consequences.
Aside from the patient registry aspect, this entire thing might only need to involve one managing pharmacist per hospital and whatever staff the system managers could hire to do analysis and make recommendations. For the registry, the data would make a highly persuasive case for a root solution or government intervention if the problem is as bad as anecdotal evidence suggests. I am always leery of data not obtained from randomized control trials, so perhaps that could be built into situations where doctors are currently forced to choose which patient gets a drug.
I’ve probably just described a more complicated system than HealthCare.gov, but this could at least be tested on a small scale, perhaps within a single hospital system (which would facilitate sharing anyway) and tracking only a few drugs to start.